Patients can now book and cancel GP appointments through a new feature launched on iPlato’s MyGP.
iPlato, which is still awaiting full integration with the systems from the principal GP providers, is pushing the new features, which also include a smoking cessation advice, in bid to bump-up patient uptake of online GP services.
Chief executive Tobias Alpsten said that while existing principal providers – EMIS, TPP, INPS and Microtest – already offer booking services, the public uptake so far has been poor.
The 2015 National GP Survey found that just 7% of patients booked an appointment online, up from 6.1% the previous year.
Only a third of patients were aware that booking online was even an option, with the majority booking by telephone and a quarter by physically dropping by their GP practice.
“The core principals will always be one step ahead, so our focus needs to on being more popular with patients,” Alpsten said. “That’s where the battle will be.”
iPlato has an established text-based alert service used by about 1,500 GP practices but has started venturing more aggressively into a health-based mobile apps in the past year.
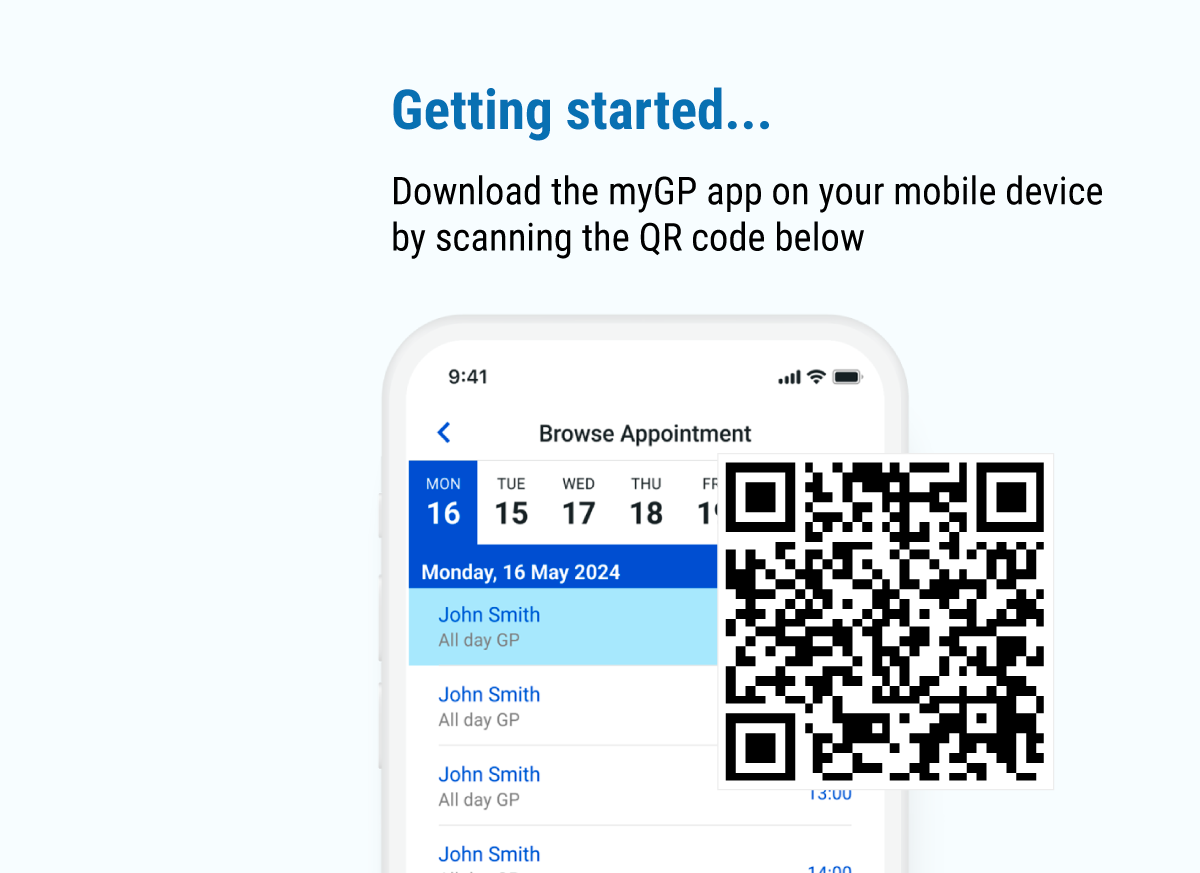
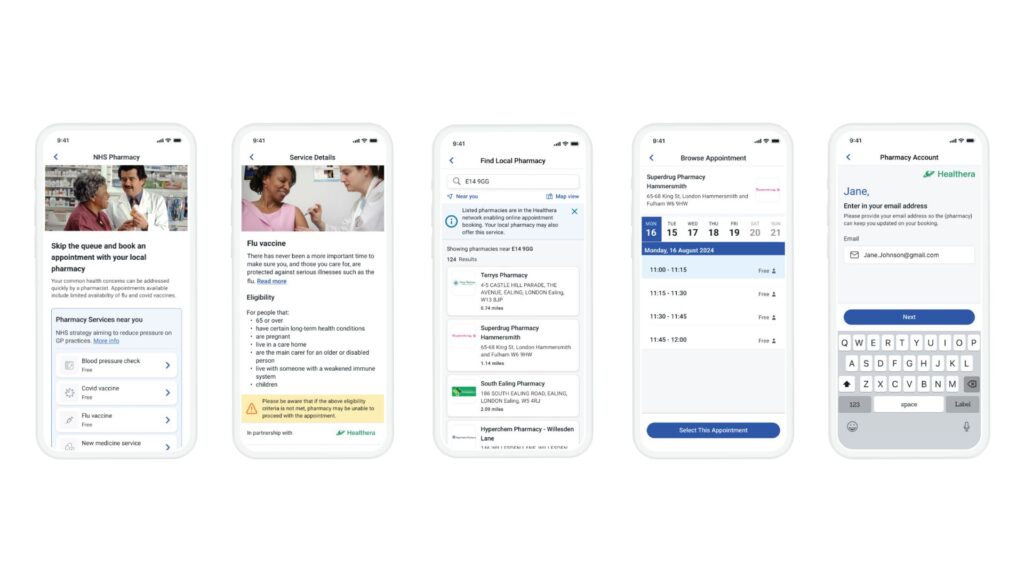
MyGP released its appointment booking through the MyGP app in May. It allows patients to remotely book and cancel GP appointments through an app on their mobile phone.
It can also register patients remotely, including asking basic health questions such as whether they are smokers, and automatically send that information back to their GP.
The app also has non-transmitting functionality for medication alerts, blood pressure monitoring and weight management, and a secure messaging service.
To date, 54 GP practices have signed up, along with 5,000 patients. In a pilot at a Kent GP practice, as many as 27% of enrolled patients signed-up to MyGP, Alpsten said. “We are trying to come up with little things that the patient wants, not what the NHS wants.”
While MyGP is aimed at customers, it will also need to get buy-in from busy GPs, many of whom view ever-expanding array of platforms for interacting with patients as too time consuming to keep on top of at a time of rapidly rising demand.
Alpsten said he believed GPs would be persuaded by the app’s ability to let patients cancel appointments, which should reduce ‘did not attends’, the medication self-management function, which should improve medication adherence, and the automatic collection of basic patient information, which should save time.
MyGP is one of several third-party providers waiting for the conclusion of negotiations between the Health and Social Care Information Centre and principal GP providers over opening up their application programming interfaces.
Open APIs would allow the suppliers of subsidiary services to integrate with core platforms. While all providers have signed up to provide better integration, progress has been slow, with the deadline pushed back repeatedly.
There are more than 50 “pairings” of principal and third party suppliers going through the HSCIC process, but just two integrations have been awarded full roll-out approval in more than 18 months.
These are Total Billing Solutions with its product Medibooks and My RightCare, which enables GPs and patients to create care plans together.
Subsidiary providers of patient facing GP services – including PAERS, Wiggly Amps and iPlato – have found the process particularly slow and challenging, but are hopeful of the end result.
“It is an incredibly long process; we were awarded the contract in 2015,” Alpsten said. In the meantime, he is banking on patient enthusiasm to push the take-up of MyGP without full interoperability with the principal providers.